The World Health Organization (WHO, 2018) estimates that approximately 15% of the world population lives with a disability. The prevalence of disability is increasing due to growth in the aging population and the number of individuals living with chronic illnesses (WHO, 2018). Disability and poverty are intricately interconnected, both serving as causes and consequences of each other (Elwan, 1999). People with disabilities often live in more impoverished circumstances than the general population (Palmer, 2011). In the United States, the percentage of people with disabilities living in poverty in 2016 was 20.9%, which is significantly higher than the percentage of people without disabilities living in poverty (13.1%; Kraus et al., 2018). The association between disability and poverty is an unfortunate cycle, as disability contributes to the risk of poverty, and poverty increases the likelihood of disability.
Disability is likely to cause or exacerbate poverty in multiple ways (Banks et al., 2017). Negative societal attitudes often result in the exclusion and marginalization of people with disabilities, further reducing the opportunity for people with disabilities to contribute productively to society and establish independence and financial stability. Consequently, they are more vulnerable to falling into poverty. In addition to attitudinal factors, there are three primary reasons people with disabilities may live in poverty at increased rates (Glendinning & Baldwin, 1988). First, many people with disabilities have a lower earning capacity than the rest of the population. Some of the reasons for this include limitations in functional capabilities, lower educational levels, physical barriers in the workplace, and lack of appropriate transportation service. Second, people with disabilities may incur extra expenses due to disability or chronic illness, including medical expenses (e.g., treatment, surgical, or pharmaceutical costs), specialized equipment, services, assistive devices, and personal assistant services. Lastly, some people with disabilities require assistance and care from other family members. As a result, the available household labor can be diminished, resulting in lower household income and even impoverished household circumstances (Elwan, 1999; Glendinning & Baldwin, 1988; Palmer, 2011).
On the other hand, people living in poverty are more vulnerable to acquiring disabilities for multiple reasons. Some poverty-related factors, such as lack of adequate access to healthcare services, inadequate nutrition, inadequate education and employment opportunities, poor household sanitation and environment, and involvement in dangerous or hazardous occupations, are more likely to result in disabilities among those living in disadvantaged situations. Particularly among people living in developing countries or rural areas, malnutrition is one of the major causes of disability, as nutrition affects health and intellectual development. Malnourished mothers may give birth to low-birth-weight babies, which is likely to increase their vulnerability to disability (Elwan, 1999; Palmer, 2011).
Since disability and poverty are closely related, health and health care access can be challenging for people with disabilities living in poverty. People with disabilities are more likely to have lower literacy rates, inadequate nutritional status, lower income levels and higher unemployment, lower immunization coverage, and lower birth weights (Banks et al., 2017). Consequently, they may have limitations in their access to healthcare resources or may not be knowledgeable about how to effectively seek healthcare services. In addition, people with disabilities living in poverty may have more limited access to health promotion and preventive services, for example, screening for breast cancer, weight monitoring, sexual health education, and other health-promoting interventions (WHO, 2018). The WHO (2018) also reported that 51% to 53% of low-income people with disabilities are unable to afford healthcare services compared to 32% to 33% of low-income people without disabilities. Untreated physical and psychological conditions can lead to poorer health (Bohman et al., 2011). Furthermore, recent statistics show that people with disabilities in the United States are more likely to engage in unhealthy behaviors, such as smoking, unhealthy eating leading to obesity, and binge drinking, than people without disabilities (Kraus et al., 2018). A smaller percentage of low-income people with disabilities engage in health-promoting behavior than more financially stable people (Meraviglia et al., 2013). All these factors are likely to increase the risk of secondary complications or chronic conditions, further decreasing the quality of life and overall health in people with disabilities living in poverty. Consequently, the presence of a combination of disability and poverty has tremendous negative impacts on the lives of disadvantaged or underserved individuals with disabilities.
Intervention studies conducted in affluent urban and suburban settings may not generalize well to rural populations or people with low socioeconomic status, limited economic resources, and limited support. A study conducted in economically deprived areas suggested that people with disabilities living in the most deprived areas tended to have poorer health outcomes, even after providing treatment, than people with disabilities living in the least disadvantaged areas (Carr et al., 2005). Even though some literature provides evidence for the association between disability and poverty, there is a paucity of reviews that have primarily focused on intervention strategies for improving the health outcomes of people with disabilities living in poverty. Therefore, it is important to identify effective interventions that may help improve health outcomes in people with disabilities who are economically disadvantaged (Tucker et al., 2012).
The objective of this study was to conduct a scoping review of the literature related to interventions for improving the health outcomes of people with disabilities who are economically disadvantaged or living in poverty. Identification of appropriate intervention strategies may help prevent secondary conditions or disabilities and improve the health status and quality of life of those who are already living with a disability.
Methods
Scoping review methodology was utilized in this study to account for the diversity of possible literature related to the topic. Scoping reviews provide an overview of a broad or complex topic. The scoping review does not attempt to evaluate the quality of research; instead, it generally describes the overall state of research or literature in the area to identify any knowledge gaps (Arksey & O’Malley, 2005). This review was guided by the scoping review framework proposed by Arksey and O’Malley (2005), including identifying the research question, selecting studies, charting and collating data, and summarizing and reporting the results. In this scoping review, the interventions or experimental literature pertaining to improving the health conditions of people with disabilities who are disadvantaged, live in poverty, or have a low socioeconomic status were analyzed and synthesized.
The following electronic databases were searched in April 2022 for studies assessing interventions aimed at improving health outcomes among people with disabilities who are poor, economically deprived, or disadvantaged: Cumulative Index to Nursing and Allied Health Literature, PsychInfo, PubMed, ERIC, and Social Science Abstracts. In addition, references of the relevant studies were checked to identify any other potential studies. The following search terms were utilized: “poverty” or “low-income” or “low socioeconomic” or “disadvantaged” AND “smoking cessation” or “health care” or “health promotion” or “health literacy” AND “disability” or “disabilities” or disabled" or “chronic illness” AND “quasi-experimental” or “single subject” or “case design” or randomized" or “pre-test.” The search was limited to studies published in English between January 2000 and April 2022 and conducted among working-age adults aged 18-64 years old.
The inclusion criteria for the selection of the articles in this review were: (1) empirical research studies, (2) tested a specific intervention, (3) measured health and well-being outcomes, (4) included individuals with disabilities or chronic illnesses with the age range between 18 and 64 years old, and (5) involved socioeconomically disadvantaged individuals as participants. Because many chronic illnesses lead to disability, studies conducted among people with chronic illnesses were also included in this review.
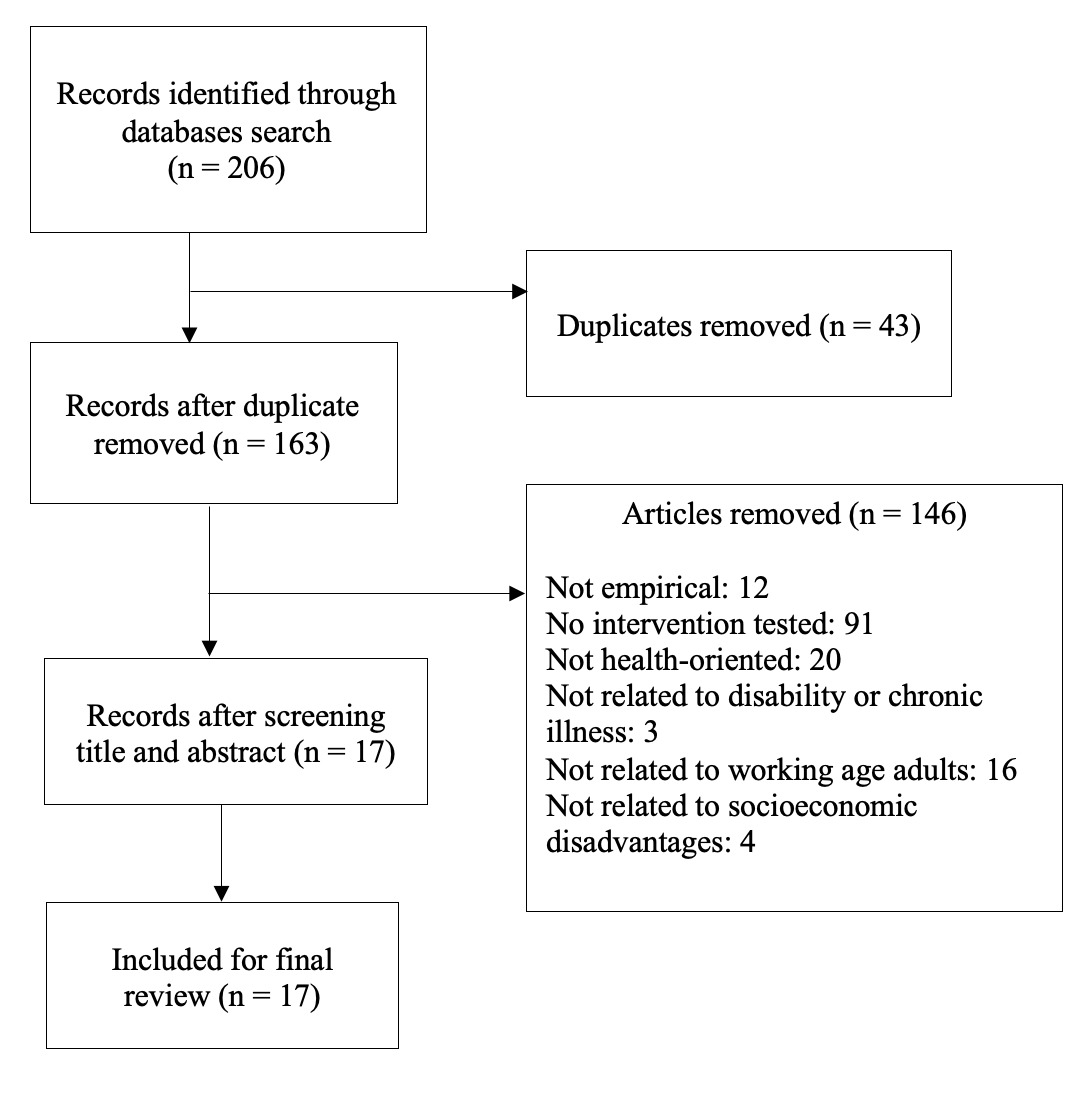
The database search took place in April 2022. The search resulted in 206 articles, of which 43 were duplicates, resulting in a final total of 163 articles. As a result of a careful review of abstracts from the 163 articles, 146 were removed for multiple reasons as follows: not empirical studies, descriptive studies, not including the working adult population, and not related to individuals living in poverty (Figure 1). Guided by the inclusion criteria, 17 articles were identified as being relevant and were retained for the final review.
Results
A total of 17 articles were included in the review, and studies were diverse in terms of population, disability conditions, targeted health outcomes, and interventions. The most common population of interest was individuals with HIV, which was the focus of five of the 17 articles (Cabral et al., 2007; Heckman & Carlson, 2007; Segal-Isaacson et al., 2006; Simoni et al., 2013; Tucker et al., 2012). Two studies included participants with serious mental illnesses (Otto-Salaj et al., 2001; Padgett et al., 2011). Other groups included individuals with chronic pain and limitations in physical functioning, neurological disabilities (e.g., spinal cord injuries [SCI], multiple sclerosis [MS]), physical and intellectual disabilities, and chronic illnesses (e.g., diabetes, hypertension, hyperlipidemia, hepatitis C, cancer). The data from the selected studies were extracted and summarized in a table. Table 1 provides a summary of each article, including the authors’ names, publication year, participants, types of interventions, outcome variables, and an overview of the findings.
Interventions
Intervention strategies were varied throughout the studies. Many of the studies used a multi-pronged approach, utilizing a variety of different types of interventions combined into a comprehensive program. Several of the intervention programs were in a group format with a clear theoretical focus (e.g., cognitive behavioral, Bandura’s self-efficacy). Carr et al. (2005) examined a group exercise program based on cognitive behavioral theory. Though the program did not cause significant improvements in participants’ disability scores, mild improvements in disability scores were noticed after three months and 12 months of intervention. Block et al. (2010) reported significant improvements in general self-efficacy after administering a 10-day intervention intended to build capacity for health promotion and independent living. Farrell et al. (2004) also reported a significant positive effect of an interactive chronic disease self-management program, which was based on Bandura’s self-efficacy theory.
Similarly, other interventions included a health coaching intervention provided by trained certified medical assistants (Thom et al., 2015), a strength-based flourishing intervention (Bu & Duan, 2021), a low barrier, multidisciplinary community-based support program (Mason et al., 2015), a seven-session small group cognitive behavioral HIV risk reduction program (Otto-Salaj et al., 2001), a line dancing intervention (Murrock et al., 2015), a three-component intervention intended to encourage health-promoting behaviors (Meraviglia et al., 2013), a culturally adapted cognitive behavioral therapy (Simoni et al., 2013), an outreach program (Cabral et al., 2007), stress management and relaxation training combined with expressive-supportive therapy (Segal-Isaacson et al., 2006), provision of stable housing (Padgett et al., 2011), information support and coping improvement group interventions (Heckman & Carlson, 2007), an interactive voice response system (Tucker et al., 2012), a walking program (Melville et al., 2015), and an employment-focused case management program (Bohman et al., 2011). Most of the interventions that were tested demonstrated improvements in the health outcomes of the population of interest over time.
Intervention Outcomes
The most common outcome of interest was self-efficacy, both general and specific to health or pain, with four of the 17 articles focusing on self-efficacy. Block et al. (2010) measured general perceived self-efficacy, Farrell et al. (2004) assessed self-efficacy influencing health along with self-management (cognitive symptoms), and other two studies examined pain self-efficacy and health promotion self-efficacy (Carr et al., 2005; Meraviglia et al., 2013). Other outcomes of interest in different studies were disability level (Carr et al., 2005; Murrock et al., 2015); resilience and flourishing (Bu & Duan, 2021); quality of life (Meraviglia et al., 2013); healthy behaviors, such as physical activity, nutrition, safe sex practices, seeking medical care, and reduced substance use (Melville et al., 2015; Otto-Salaj et al., 2001; Padgett et al., 2011; Segal-Isaacson et al., 2006; Tucker et al., 2012); mental health (Heckman & Carlson, 2007; Mason et al., 2015; Simoni et al., 2013); satisfaction with medical care (Cabral et al., 2007; Thom et al., 2015); and employment outcomes (Bohman et al., 2011; Mason et al., 2015).
Discussion
The scoping review of 17 articles identified various interventions for improving health and well-being outcomes in people with chronic illnesses and disabilities living in poverty. All the selected studies were heterogeneous in terms of the nature of participants, interventions, and outcomes. The results demonstrated that a wide array of intervention strategies could be utilized to improve various health-related outcomes among people with different chronic illnesses and disabilities. This review sheds light on some strategies that can help improve general and specific self-efficacy, self-management ability, resilience, quality of life, physical activity, healthy behaviors, safe-sex practices, and many other health-related outcomes. Many of the interventions are based on well-established theories, such as Bandura’s self-efficacy theory, cognitive behavioral theory, Pender’s health promotion theory, and well-being theory (Bu & Duan, 2021; Carr et al., 2005; Farrell et al., 2004; Heckman & Carlson, 2007; Meraviglia et al., 2013; Otto-Salaj et al., 2001; Segal-Isaacson et al., 2006; Simoni et al., 2013). The programs that were developed utilizing these theories can be modified based on the context and types of disabilities and implemented with different populations. Preventing further disability is crucial to promoting a better quality of life for people who have already sustained some form of disability. Hence, applying health promotion interventions will likely enhance the health status and the quality of life of disadvantaged adults with disabilities.
Rehabilitation counselors can consider replicating or implementing some of the interventions identified in this review. Block et al. (2010) examined an intervention among people with neurological impairments such as spinal cord injury and multiple sclerosis. Their intervention was found to help improve the participants’ health and quality of life. The intervention consisted of 10 days of meetings for five months with interactive workshops on health promotion and independent living topics, accessible physical and recreational activities, and peer mentoring. Though this program was examined among people with neurological impairments, it may be effective for other disabilities and chronic illnesses. Among people with disabilities, environmental or attitudinal barriers (e.g., lack of architectural structures, societal stigma, and discrimination) are commonly identified barriers on top of disability-related impairments. This program works by modifying the environment by means of assistive technology, promoting self-advocacy to get needs met, and encouraging participation in community life (Block et al., 2010). This type of intervention promotes independence and access to the community through education and advocacy, which may be applicable to individuals with many different types of disabilities. Strength-based flourishing interventions can also be utilized to promote resilience and, thus, positive adaptation (Bu & Duan, 2021).
Similarly, Segal-Issacson et al. (2006) administered a nutrition education intervention to disadvantaged women with HIV/AIDS and found that it was effective in improving dietary patterns among participants. Healthy dietary behaviors are crucial to maintaining physical and mental health among all people, particularly those with disabilities. To improve healthy dietary behaviors, a nutrition intervention such as the one examined in the study might be beneficial for people with different disabilities. In addition, a health promotion intervention program consisting of multiple components—individual counseling related to health-promoting behavior, classes on adopting and practicing health-promoting behavior, and follow-up support—was found to be promising to improve healthy behaviors (Meraviglia et al., 2013). Hence, rehabilitation practitioners can adapt and implement such interventions by encouraging people with disabilities to adopt health-promoting behavior by emphasizing the potential benefits of such behavior.
Other interventions, such as those related to physical fitness, can be considered on a community level or even in rehabilitation centers. Murrock et al. (2015) reported the effectiveness of a dance and exercise intervention in improving upper extremities functioning. Immobility is one of the major limitations following the onset of physical disabilities such as stroke, SCI, MS, chronic pain, and many others. Such exercises are evidenced to be effective for strengthening the muscles of the upper and lower extremities and improving mobility. As a result, individuals with disabilities may be able to maintain functioning and, in turn, contribute to their economic stability and independent living success in the future.
Some interventions reported non-significant findings, and other interventions may raise the questions of feasibility and generalizability. Carr et al. (2005) suggested that even though the group exercise program does not differ significantly from an individual physiotherapy program, group therapy is less costly than individual therapy. Therefore, the authors argue that group therapy should be considered as an alternative to expensive individual physiotherapy. Their comprehensive Working Well intervention program addressed the health, employment, and social needs of uninsured working individuals in Texas. This three-year program was found to be effective in improving health care utilization and satisfaction with health care (Bohman et al., 2011); however, such a long-term comprehensive program may not be feasible for low- or middle-income individuals. Therefore, a more cost- and time-effective program is needed in such cases.
In addition, some interventions might not be effective due to the challenging nature of the disability. Melville et al. (2015) implemented an intervention with the goal of increasing walking and reducing sedentary behavior in adults with intellectual disabilities. The program did not yield significant changes in behavior. The researchers argued that adopting complex behavior changes is challenging for people with intellectual disabilities. Usually, people with intellectual disabilities are supported by family members or caregivers in decision-making, and it is difficult to find time to work together with clients and caregivers. Such a program may not be generalizable to families who experience multiple social disadvantages. Therefore, a more intensive program focusing on changing the knowledge and behavior of caregivers might be more effective.
The review identified some gaps in the present literature. Even though there is a growing number of interventional studies among people with chronic illnesses and disabilities, disadvantaged or underserved people with disabilities have gained relatively little attention. Those populations may be more likely to have unhealthy behaviors and less likely to receive health promotion interventions (WHO, 2018). Carr et al. (2005) identified differences in disability scores among people in the most and least deprived areas. The authors also noted that even after health-promoting interventions were provided, participants from the most severely deprived areas reported low disability scores at follow-up, whereas participants from the least deprived or more affluent areas were likely to experience improvements in their disability scores. This result reflects the need to give emphasis to people in poor or deprived circumstances. It is necessary to adapt treatment approaches to the needs of different socioeconomic groups. Melville et al. (2015) pointed out that interventions to change the health behaviors of disadvantaged people with disabilities are one of the ways to reduce health disparities and improve health outcomes. Another gap identified in the literature is that all the intervention strategies were different and such interventions were tested only in a single study and with people with a specific disability. This might raise the question of the reliability or effectiveness of the interventions in other groups.
Overall, it is evident from the current review that the health outcomes of people with disabilities living in poverty can be improved using some interventions or programs; however, further studies are indicated. Out of 17 studies reviewed, five studies were conducted among people with HIV/AIDS. Some attention has been given to people with intellectual and physical disabilities, as well. Health promotion interventions will need to be adapted to the cognitive level of individuals with intellectual disabilities. Similarly, interventions conducted among individuals with chronic illnesses may not be applicable to people with certain mobility limitations. Therefore, more studies are needed in this area to develop appropriate interventions tailored specifically to the needs of individuals with different disabilities in order to improve their health outcomes.
The findings of this review need to be interpreted in light of some limitations. The authors conducted a scoping review rather than a systematic review to gather a wide range of literature. A limitation of this approach could be that the review included all the relevant studies regardless of the quality of the research. Yet, the literature in this area is limited, and this review aimed to glean evidence for improving health outcomes for people with disabilities who are disadvantaged. Though the quality of studies was not assessed, all the selected studies were empirical. Another limitation could be that the review included the studies published after the year 2000. Hence, the review may not consider all the effective interventions or strategies that were studied before the year 2000. The review included a wide range of studies with diverse health/disability conditions, contexts, interventions, and outcome measures. Therefore, it is crucial to overview the limitations of those interventions while generalizing the findings.
Conclusion
The scoping review identified many interventions for people with disabilities living in poverty. Given the disparate nature of the articles included in this review, it is clear that more work needs to be done in developing and testing interventions to improve health and well-being outcomes for this group. The only group of individuals who received more than cursory attention is individuals with HIV. Even then, only five articles were identified that empirically tested interventions to improve health outcomes in that population. Many studies conducted in this area are cross-sectional descriptive designs. Therefore, research in rehabilitation should increase its focus on intervention testing to ensure that empirically sound interventions become available to improve health outcomes in individuals with chronic illnesses and disabilities living in poverty.
Funding
The contents of this article were developed with support from the Vocational Rehabilitation Technical Assistance Center for Quality Employment, H264K200003, and the Vocational Rehabilitation Technical Assistance Center for Targeted Communities, H264F15003, from the U.S. Department of Education. However, the contents do not necessarily represent the policy of the U.S. Department of Education, and you should not assume endorsement by the Federal government.